
analgesic and/or an anxiolytic is recommended. In addition to 1% lidocaine injected around the incision site to reduce pain, premedication with an I.V. As part of your safety and contingency preparations, keep petroleum gauze and a rubber-tipped clamp at the patient’s bedside, especially during transfers, in case of complications.Īntibiotic and pain prophylaxis: Antibiotic prophylaxis is recommended only for patients with traumatic chest injuries. For underwater seal CDUs, the most important preparation is filling the water seal chamber with sterile water or sterile normal saline to the prescribed level (2 cm). (See Small bore or large bore?) Set up chest drainage units (CDUs) per the manufacturer’s recommendations. Gather supplies: As ordered by the provider, prepare the CTT insertion tray, tube, and drainage system. You’ll also be involved in gathering supplies, administering antibiotic and pain prophylaxis as ordered, assisting with selecting and imaging the insertion site, positioning the patient, ensuring sterile technique, securing the tube, and confirming placement. Anticoagulant use is a relative contraindication to CTT insertion, but the provider will weigh the risks and benefits. Hemorrhage is a potential complication of chest tube placement, so review the patient’s medications (look for heparin, warfarin, apixaban) and coagulation profile (activated partial prothrombin time, international normalized ratio, platelets, and fibrinogen). Taking these steps will improve patient cooperation during the procedure.
Explain the procedure to the patient, assess his or her comprehension, answer questions within your purview, and allow the patient to express his or her anxiety. When a provider orders a CTT, your responsibilities include verifying patient identification, ascertaining that informed consent has been obtained (except in emergencies), and determining patient understanding of the procedure. CTTs drain fluid and air in the pleural cavity to promote lung re-expansion.

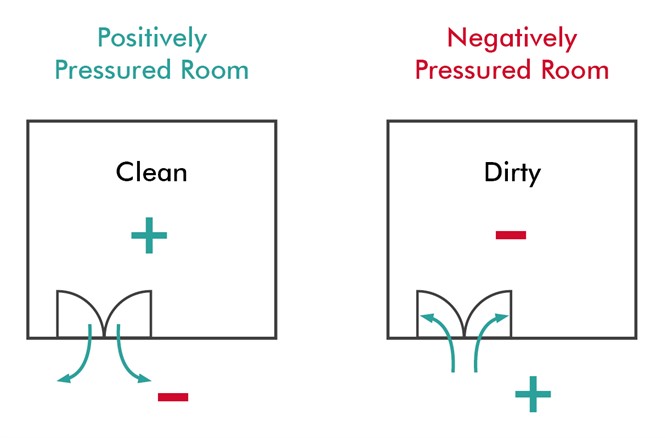
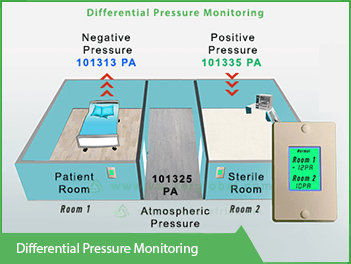
An extreme case is tension pneumothorax, which is characterized by progressive accumulation and trapping of air in the pleural cavity, causing pressure buildup that obliterates space for adjacent structures (lungs, vena cava, and heart). The body can handle small amounts of extra pleural fluid or air, but large amounts (≥ 300 mL) impede ventilation. When pleural integrity is breached, excess blood, serous fluid, or air accumulates. The decreased size of the lungs reverses the pressure gradient, and air is forced out into the atmosphere.īetween the outer lining of the lungs and the inner chest wall lies the pleural space, which normally is lubricated by pleural fluid in the amount of 0.2 mL/kg (10 to 20 mL for average-size adults). The second part of ventilation, exhalation, is passive as the diaphragm and other respiratory muscles resume their resting configuration. Air moves from the atmosphere of greater pressure and into the thoracic cavity, where pressure is lower. The chest cavity expands, mostly through diaphragm contraction, lowering pressure inside the chest cavity and effectively creating suction. Ventilation, a two-part process, begins with inhalation. Understanding CTTs begins with understanding how breathing works. CTTs can be life-saving, but only if managed based on current best evidence.


 0 kommentar(er)
0 kommentar(er)
